|
| Head Injury |
Supratentorial Tumors |
Posterior Fossa Surgery|
Intracranial Aneurysms
|Ischemic Cerebrovascular Diseases
|Neuroendocrine Tumors
|Epilepsy-Awake
Craniotomy-Intraoperative MRI
|Spinal Cord Injury and Procedures
|Pediatric Neuroanesthesia
|Neurosurgery in the Pregnant
Patient
|Management of Therapeutic
Interventional Neuroradiology
|Management in Diagnostic
Neuroradiology
|

The endovascular approach has opened new options in
the treatment of vascular and nonvascular
intracranial and spinal diseases. Interventional
neuroradiologic (INR) procedures may seem
technically straightforward, yet they carry a
significant morbidity. Approximately 0.2% to 1% of
the patients develop transient or permanent
neurologic signs and symptoms after diagnostic
cerebral angiography. When compared with diagnostic
angiography, therapeutic interventions are
associated with significantly more risks of
neurologic complications. The primary goals of
anesthesia for INR procedures are to control the
level of sedation in a manner that permits prompt
neurologic examination, to render the patient
immobile, and to manipulate cerebral hemodynamics.
Many INR procedures such as diagnostic angiography,
carotid angioplasty and stenting (CAS), and
embolization of cerebral arteriovenous malformations
(AVMs) can be undertaken with intravenous sedation.
General anesthesia is required, however, for a
growing number of INR procedures including
intracranial angioplasty and embolization of
aneurysms and some high-flow AVMs, diagnostic
procedures in children and uncooperative adults, and
prolonged procedures such as those on the spinal
cord. Often the choice of anesthetic technique is a
collaborative decision by the radiologist and the
anesthesiologist on the basis of their assessment of
each individual patient.
I. Neurovascular
access and methods
 Vascular access.
INR procedures typically involve the insertion of
catheters into the arterial circulation of the head
or the neck, usually through the transfemoral route.
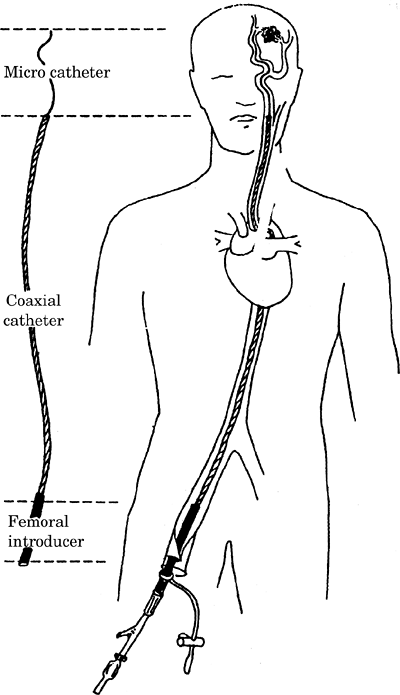
As illustrated in Figure-1, transfemoral arterial
access is accomplished by the placement of a large
introducer sheath into the femoral artery, usually 5
to 7.5 Fr in size. A 5 to 7.5 Fr coaxial catheter is
positioned through the introducer sheath into either
the carotid or vertebral artery by fluoroscopic
control. Finally, a 1.5 to 2.8 Fr superselective
microcatheter is introduced into the cerebral
circulation to deliver drugs, embolic agents, or
balloons to distal regions of the brain. The
transfemoral placement site is usually infiltrated
with a local anesthetic, which can cause femoral
nerve block and a temporary weakness of the
quadriceps muscle. Transfemoral venous access can
also be used to reach the dural sinuses and, in some
cases, the arterial side of an AVM. Direct
percutaneous puncture is used to access superficial
lesions of the head and neck, such as tumors and
arteriovenous and venous malformations.
Vascular access.
INR procedures typically involve the insertion of
catheters into the arterial circulation of the head
or the neck, usually through the transfemoral route.
As illustrated in Figure-1, transfemoral arterial
access is accomplished by the placement of a large
introducer sheath into the femoral artery, usually 5
to 7.5 Fr in size. A 5 to 7.5 Fr coaxial catheter is
positioned through the introducer sheath into either
the carotid or vertebral artery by fluoroscopic
control. Finally, a 1.5 to 2.8 Fr superselective
microcatheter is introduced into the cerebral
circulation to deliver drugs, embolic agents, or
balloons to distal regions of the brain. The
transfemoral placement site is usually infiltrated
with a local anesthetic, which can cause femoral
nerve block and a temporary weakness of the
quadriceps muscle. Transfemoral venous access can
also be used to reach the dural sinuses and, in some
cases, the arterial side of an AVM. Direct
percutaneous puncture is used to access superficial
lesions of the head and neck, such as tumors and
arteriovenous and venous malformations.
|
Figure-1. Representation
of a typical arrangement of a transfemoral
coaxial catheter system showing the femoral
introducer sheath, the coaxial catheter, and
the microcatheter. |
|
 |
 Imaging technology.
Radiologic imaging techniques needed for INR
procedures include high-resolution fluoroscopy and
high-speed digital subtraction angiography (DSA)
with road-mapping functions. DSA enables the
visualization of only those vessels that are
opacified by contrast injection. The road-mapping
function enables the radiologist to observe the
advance of the catheter against the background map
of the patient's cerebral vessels "in real time."
DSA involves subtraction of the images obtained
before and after the injection of the radiocontrast
drug. Any displacement of the cerebral vessels
because of the movement of the head profoundly
degrades the DSA images. Hence, it is critical that
the patient remain immobile during the procedure.
Imaging technology.
Radiologic imaging techniques needed for INR
procedures include high-resolution fluoroscopy and
high-speed digital subtraction angiography (DSA)
with road-mapping functions. DSA enables the
visualization of only those vessels that are
opacified by contrast injection. The road-mapping
function enables the radiologist to observe the
advance of the catheter against the background map
of the patient's cerebral vessels "in real time."
DSA involves subtraction of the images obtained
before and after the injection of the radiocontrast
drug. Any displacement of the cerebral vessels
because of the movement of the head profoundly
degrades the DSA images. Hence, it is critical that
the patient remain immobile during the procedure.
 Materials for embolization
and infusion. Factors that affect the
choice of the embolic agent include the nature of
the disease, the purpose of embolization, the size
and penetration of emboli and vessels, and the
permanency of occlusion. The ideal choice and the
combination of agents remain controversial. Embolic
agents include balloons, coils, polyvinyl alcohol
(PVA) particles, gelatinous embolization spheres,
and glue. As used for embolization, N-butyl
cyanoacrylate (NBCA) glue is available as a liquid
monomer that rapidly polymerizes in contact with
ionic solutions such as blood and saline.
Materials for embolization
and infusion. Factors that affect the
choice of the embolic agent include the nature of
the disease, the purpose of embolization, the size
and penetration of emboli and vessels, and the
permanency of occlusion. The ideal choice and the
combination of agents remain controversial. Embolic
agents include balloons, coils, polyvinyl alcohol
(PVA) particles, gelatinous embolization spheres,
and glue. As used for embolization, N-butyl
cyanoacrylate (NBCA) glue is available as a liquid
monomer that rapidly polymerizes in contact with
ionic solutions such as blood and saline.
II. Anesthetic
considerations
Briefly, the primary functions of
the anesthesiologist in the intervention suite are
(a) to provide to the patient the level of sedation
that permits prompt neurologic assessment when
needed, (b) to render the patient physiologically
stable and immobile, (c) to manipulate systemic
blood pressure optimally as dictated by the needs of
the procedure, and (d) to provide emergent
management of catastrophic complications.
III. Conduct of
anesthesia for INR procedures
 Preoperative assessment.
A careful assessment of the airway must be made. A
history of snoring may suggest that partial airway
obstruction might occur with sedation. Snoring
results in movement artifacts that may degrade the
quality of images during cerebral angiography.
Patients who have a history of adverse reaction to
radiocontrast drugs require pretreatment with
steroids and antihistaminic drugs. The population of
patients who have occlusive cerebrovascular disease
might also require adequate treatment of
hypertension, heart failure, or angina. Preoperative
communication should exist with the INR team to
develop a clear strategy for sedation and
hemodynamic interventions that might be needed
during the procedure.
Preoperative assessment.
A careful assessment of the airway must be made. A
history of snoring may suggest that partial airway
obstruction might occur with sedation. Snoring
results in movement artifacts that may degrade the
quality of images during cerebral angiography.
Patients who have a history of adverse reaction to
radiocontrast drugs require pretreatment with
steroids and antihistaminic drugs. The population of
patients who have occlusive cerebrovascular disease
might also require adequate treatment of
hypertension, heart failure, or angina. Preoperative
communication should exist with the INR team to
develop a clear strategy for sedation and
hemodynamic interventions that might be needed
during the procedure.
 Preoperative
investigations. The routine guidelines
for indicated laboratory investigations before
surgery are applicable to INR procedures. Of
particular interest is the baseline coagulation
screen because anticoagulation is required for the
procedure.
Preoperative
investigations. The routine guidelines
for indicated laboratory investigations before
surgery are applicable to INR procedures. Of
particular interest is the baseline coagulation
screen because anticoagulation is required for the
procedure.
 Premedication.
Anxiolytics may be administered depending on the
condition of the patient. Minimal premedication is
required for INR procedures. Either oral nimodipine
or transdermal nitroglycerin is sometimes used to
decrease intraoperative vasospasm.
Premedication.
Anxiolytics may be administered depending on the
condition of the patient. Minimal premedication is
required for INR procedures. Either oral nimodipine
or transdermal nitroglycerin is sometimes used to
decrease intraoperative vasospasm.
 Room preparation.
The INR suite should have the same anesthesia
equipment as is available in a standard operating
room. Suction, gas evacuation, oxygen, and nitrous
oxide (N2O) should be available from the
wall outlets. Ideally, the anesthesia machine should
have the capacity to provide carbon dioxide (CO2)
for deliberate hypercapnia. An extended anesthetic
breathing system is necessary to reach the remotely
located patient's airway. Rapid access to all
critical equipment should be possible at all times
during the procedure. Induction and emergency drugs
must be prepared and ready for immediate use.
Room preparation.
The INR suite should have the same anesthesia
equipment as is available in a standard operating
room. Suction, gas evacuation, oxygen, and nitrous
oxide (N2O) should be available from the
wall outlets. Ideally, the anesthesia machine should
have the capacity to provide carbon dioxide (CO2)
for deliberate hypercapnia. An extended anesthetic
breathing system is necessary to reach the remotely
located patient's airway. Rapid access to all
critical equipment should be possible at all times
during the procedure. Induction and emergency drugs
must be prepared and ready for immediate use.
 Patient positioning.
Because INR procedures may last for several hours,
it is essential that the patient be made as
comfortable as possible before the start of
sedation.
Patient positioning.
Because INR procedures may last for several hours,
it is essential that the patient be made as
comfortable as possible before the start of
sedation.
 Intravenous access. During INR procedures,
patients are often moved cephalad toward the image
intensifier and away from the anesthesiologist to
check the position of the catheters. This limits
access to venipuncture sites and injection ports
during the procedure. Therefore, adequate vascular
access and a sufficient length of intravenous tubing
should be in place before the start of the
procedure. In adults, two intravenous cannulae are
usually inserted for this purpose; one cannula is at
least 18 gauge in size. The anesthetic and
vasoactive drugs should be in line before the
patient is draped.
Intravenous access. During INR procedures,
patients are often moved cephalad toward the image
intensifier and away from the anesthesiologist to
check the position of the catheters. This limits
access to venipuncture sites and injection ports
during the procedure. Therefore, adequate vascular
access and a sufficient length of intravenous tubing
should be in place before the start of the
procedure. In adults, two intravenous cannulae are
usually inserted for this purpose; one cannula is at
least 18 gauge in size. The anesthetic and
vasoactive drugs should be in line before the
patient is draped.
 Monitoring
Monitoring
 Arterial pressure.
Because of the need to manipulate systemic
hemodynamics and the emergent need, at times, for
hemodynamic interventions, it is usually desirable
to obtain direct measurement of systemic arterial
pressure during INR procedures. This is most
conveniently achieved by transducing the side arm of
the femoral introducer sheath. If a relatively large
coaxial catheter passes through the introducer,
however, the arterial pressure trace is "damped."�
Despite damping, the mean pressure is still reliable
in this situation. To avoid excessive damping of the
femoral arterial trace, the introducer sheath should
be at least 0.5 Fr larger than the coaxial catheter.
Radial artery cannulation may be desirable when
systemic arterial pressure needs to be monitored
before inserting the femoral introducer sheath.
Radial arterial line may be required during the
induction of general anesthesia for the coil
occlusion of an intracranial aneurysm or when
monitoring blood pressure in the postoperative
period is indicated.
Arterial pressure.
Because of the need to manipulate systemic
hemodynamics and the emergent need, at times, for
hemodynamic interventions, it is usually desirable
to obtain direct measurement of systemic arterial
pressure during INR procedures. This is most
conveniently achieved by transducing the side arm of
the femoral introducer sheath. If a relatively large
coaxial catheter passes through the introducer,
however, the arterial pressure trace is "damped."�
Despite damping, the mean pressure is still reliable
in this situation. To avoid excessive damping of the
femoral arterial trace, the introducer sheath should
be at least 0.5 Fr larger than the coaxial catheter.
Radial artery cannulation may be desirable when
systemic arterial pressure needs to be monitored
before inserting the femoral introducer sheath.
Radial arterial line may be required during the
induction of general anesthesia for the coil
occlusion of an intracranial aneurysm or when
monitoring blood pressure in the postoperative
period is indicated.
During a typical intracranial INR procedure, two
other pressures may be measured in real time in
addition to the systemic arterial pressure: either
the internal carotid or vertebral artery pressure
through the coaxial catheter or the distal cerebral
arterial pressure through either the microcatheter
or a balloon-tipped catheter. The coaxial catheter
pressure is monitored to detect either thrombus
formation or vasospasm at the catheter tip as
evidenced by a damped arterial trace. A high volume
of heparinized flush solution is infused
continuously through the coaxial tip to discourage
thrombus formation; hence, the pressure reading
characteristically increases by 10 to 20 mm Hg when
recorded through the coaxial catheter. The setup for
measuring arterial pressures is shown in Figure-2.
The pressure transducers and access stopcocks for
zeroing and withdrawal of blood are mounted,
depending on the institutional preferences, either
on the sterile field or toward the anesthesiologist.
Measurements of the distal cerebral arterial
pressure made through the microcatheter are useful
during embolization of AVMs. When a balloon-tipped
catheter is used for internal carotid artery (ICA)
occlusion, pressure measurements at the tip of the
catheter provide the stump pressure.
|
Figure-2. Schematic
representation of pressure monitoring and
the continuous flush systems. |
|
 |
 Other systemic monitoring. Other monitors include
five-lead electrocardiogram, preferably with ST
segment trending and respiratory trace, automated
blood pressure, end-tidal CO2, and peripheral
temperature probe. Pulse oximeter probes are placed
on each of the great toes and are useful for
qualitatively comparing distal pulses in the lower
limbs. Loss of the oximeter pulse trace on the side
of the femoral introducer sheath might provide an
early warning of the occurrence of thromboembolism,
vasospasm, or mechanical obstruction.
Other systemic monitoring. Other monitors include
five-lead electrocardiogram, preferably with ST
segment trending and respiratory trace, automated
blood pressure, end-tidal CO2, and peripheral
temperature probe. Pulse oximeter probes are placed
on each of the great toes and are useful for
qualitatively comparing distal pulses in the lower
limbs. Loss of the oximeter pulse trace on the side
of the femoral introducer sheath might provide an
early warning of the occurrence of thromboembolism,
vasospasm, or mechanical obstruction.
 Central nervous system (CNS) monitoring. During many
procedures, neurologic examination provides adequate
monitoring of the integrity of the CNS. Adjuncts
especially useful during general anesthesia or
planned proximal occlusions include
electroencephalogram, somatosensory and motor evoked
potentials, transcranial Doppler (TCD) ultrasound,
and 133Xe cerebral blood flow (CBF) monitoring.
Central nervous system (CNS) monitoring. During many
procedures, neurologic examination provides adequate
monitoring of the integrity of the CNS. Adjuncts
especially useful during general anesthesia or
planned proximal occlusions include
electroencephalogram, somatosensory and motor evoked
potentials, transcranial Doppler (TCD) ultrasound,
and 133Xe cerebral blood flow (CBF) monitoring.
 Urinary output. Most patients undergoing INR
procedures require catheterization of the bladder to
assist in fluid management and to increase their
level of comfort. Diuresis may also occur during the
procedure from the increase in intravascular volume
attendant upon continuous flushing of the
intravascular lines and from the osmotic load
conferred by the injection of either mannitol or the
radiocontrast drug. The timing and volume of the
injected radiocontrast need to be monitored,
especially during prolonged procedures.
Urinary output. Most patients undergoing INR
procedures require catheterization of the bladder to
assist in fluid management and to increase their
level of comfort. Diuresis may also occur during the
procedure from the increase in intravascular volume
attendant upon continuous flushing of the
intravascular lines and from the osmotic load
conferred by the injection of either mannitol or the
radiocontrast drug. The timing and volume of the
injected radiocontrast need to be monitored,
especially during prolonged procedures.
 Laboratory tests. A baseline arterial blood gas at
the time of initial arterial puncture is useful to
assess the gradient between the arterial oxygen
tension (Pao2) and the hemoglobin saturation (Sao2)
and between the arterial CO2 tension (Paco2) and the
end-tidal CO2 (ETco2). The activated clotting time
(ACT) is used to monitor coagulation. The patients
receive large volumes of fluid and radiocontrast and
can diurese considerably, so that determination of a
baseline hematocrit is helpful as well.
Laboratory tests. A baseline arterial blood gas at
the time of initial arterial puncture is useful to
assess the gradient between the arterial oxygen
tension (Pao2) and the hemoglobin saturation (Sao2)
and between the arterial CO2 tension (Paco2) and the
end-tidal CO2 (ETco2). The activated clotting time
(ACT) is used to monitor coagulation. The patients
receive large volumes of fluid and radiocontrast and
can diurese considerably, so that determination of a
baseline hematocrit is helpful as well.
 Dynamic sedation. The primary goals guiding the
choice of anesthetic for conscious sedation are
anxiolysis, the alleviation of pain and discomfort,
and the assurance of patient immobility. At the same
time, the anesthesiologist must provide for a rapid
decrease in the level of sedation when neurologic
testing is required. The procedures are not
generally painful with the exception of sclerotherapy and chemotherapy. However, an element
of pain is associated with distention of and
traction on the vessels; the injection of contrast
into the carotid artery is frequently described as "burning."� Discomfort
might also be caused by prolonged periods of
immobilization, bladder catheterization, and, to a
lesser extent, the femoral puncture site. The
patient might find the procedure psychologically
stressful because of the potential risk of stroke
during the procedure. However, immobilization of the
patient, whether by conscious effort or deep
sedation, is essential. Movement not only degrades
the quality of the images but can also result in
vascular injury.
Dynamic sedation. The primary goals guiding the
choice of anesthetic for conscious sedation are
anxiolysis, the alleviation of pain and discomfort,
and the assurance of patient immobility. At the same
time, the anesthesiologist must provide for a rapid
decrease in the level of sedation when neurologic
testing is required. The procedures are not
generally painful with the exception of sclerotherapy and chemotherapy. However, an element
of pain is associated with distention of and
traction on the vessels; the injection of contrast
into the carotid artery is frequently described as "burning."� Discomfort
might also be caused by prolonged periods of
immobilization, bladder catheterization, and, to a
lesser extent, the femoral puncture site. The
patient might find the procedure psychologically
stressful because of the potential risk of stroke
during the procedure. However, immobilization of the
patient, whether by conscious effort or deep
sedation, is essential. Movement not only degrades
the quality of the images but can also result in
vascular injury.
Anesthetic drugs are selected to achieve controlled
sedation, adequate analgesia and desired immobility.
The primary approach to conscious sedation is to
establish a base of neuroleptic anesthesia by the
titration of fentanyl, 2 to 4 mcg/kg; droperidol,
2.5 to 5 mg; and midazolam, 3 to 5 mg, after
intravenous access and monitoring have been
established and oxygen administration has begun. In
men, a small bolus of propofol is useful just as the
urinary catheter is passed. The bolus dose of
propofol also helps the anesthesiologist to assess
the patency of the airway under deep sedation and
determine whether a nasopharyngeal airway is
required. The insertion of the nasopharyngeal airway
after anticoagulation can result in troublesome
bleeding and is best avoided.
When the patient is in final position, draping is
begun and an infusion of propofol is started at a
very low dose of 10 to 20 mcg/kg/minute and then
increased slowly to render the patient immobile yet
breathing spontaneously. The recent availability of
the alpha2 agonist, dexmedetomidine, offers an
alternative to propofol and has the advantage of
improved maintenance of the airway during sedation.
Dexmedetomidine, administered as a loading dose of
0.5 to 1 mcg/kg over 20 minutes followed by an
infusion of 0.01 to 1 mcg/kg/hour also permits
neurologic examination during awake craniotomy. Some
evidence, however, indicates that the recovery of
cognitive functions might be delayed in patients
after receiving dexmedetomidine during INR
procedures. Further, patients who have received this
drug tend to have lower blood pressures in the
recovery period. This may not be desirable in
patients who are critically dependent on the
maintenance of adequate perfusion pressure to the
collateral circulation. Therefore, the choice of
anesthetics is on the basis of the experience of the
anesthesiologist, the needs of the patient, and the
requirements of the procedure.
 General anesthesia with endotracheal intubation.
General anesthesia with endotracheal intubation in
the INR suite is similar to that in the operating
room for both adult and pediatric patients. The
primary reason for employing general anesthesia is
to
reduce motion artifact and improve the quality of
the images. This is especially pertinent to the INR
treatment of spinal pathology during which extensive
multilevel angiography is sometimes performed. In
view of the fact that chest excursion during
positive-pressure ventilation can interfere with
road mapping, radiologists frequently request
periods of apnea during DSA for certain procedures;
this can best be accomplished with endotracheal
anesthesia. A theoretic' argument can be made in the
context of INR for eschewing the use of N2O because
of the possibility of expanding the volume of air
emboli introduced into the cerebral circulation.
General anesthesia with endotracheal intubation.
General anesthesia with endotracheal intubation in
the INR suite is similar to that in the operating
room for both adult and pediatric patients. The
primary reason for employing general anesthesia is
to
reduce motion artifact and improve the quality of
the images. This is especially pertinent to the INR
treatment of spinal pathology during which extensive
multilevel angiography is sometimes performed. In
view of the fact that chest excursion during
positive-pressure ventilation can interfere with
road mapping, radiologists frequently request
periods of apnea during DSA for certain procedures;
this can best be accomplished with endotracheal
anesthesia. A theoretic' argument can be made in the
context of INR for eschewing the use of N2O because
of the possibility of expanding the volume of air
emboli introduced into the cerebral circulation.
 Anticoagulation. Careful management of coagulation
is required to prevent thromboembolic complications
from the presence of catheters, which act as foreign
bodies, and from endothelial injury associated with
the passage of microcatheters. After insertion of
the femoral introducer sheath, a baseline ACT is
obtained. Heparin, 2,000 to 5,000 U/70 kg, is given
intravenously and another ACT is measured
approximately 3 to 5 minutes later. The target ACT
depends on the clinical needs and could be two to
three times the baseline value. Additional heparin
may be required throughout the procedure to maintain
adequate anticoagulation. On occasions, at the
completion of the INR procedure, heparin's
anticoagulant effect is reversed with protamine, and
the femoral artery catheter is removed in the
angiography suite. The proliferation of percutaneous
closure devices has improved hemostasis at the
arteriotomy site, particularly in patients receiving
thrombolytic and antiplatelet drugs.
Anticoagulation. Careful management of coagulation
is required to prevent thromboembolic complications
from the presence of catheters, which act as foreign
bodies, and from endothelial injury associated with
the passage of microcatheters. After insertion of
the femoral introducer sheath, a baseline ACT is
obtained. Heparin, 2,000 to 5,000 U/70 kg, is given
intravenously and another ACT is measured
approximately 3 to 5 minutes later. The target ACT
depends on the clinical needs and could be two to
three times the baseline value. Additional heparin
may be required throughout the procedure to maintain
adequate anticoagulation. On occasions, at the
completion of the INR procedure, heparin's
anticoagulant effect is reversed with protamine, and
the femoral artery catheter is removed in the
angiography suite. The proliferation of percutaneous
closure devices has improved hemostasis at the
arteriotomy site, particularly in patients receiving
thrombolytic and antiplatelet drugs.
 Deliberate hypotension. Two primary indications for
deliberate hypotension are to decrease blood flow
through an arteriovenous fistula during the
injection of glue and to test the cerebrovascular
reserve of the patient undergoing carotid occlusion.
In most instances, the level of sedation is
decreased to permit neurologic examination during
the period of deliberate hypotension. The induction
of hypotension in awake or minimally sedated
patients can be fairly challenging because large
doses of hypotensive drugs may be required to reduce
the blood pressure in these patients.
Adrenergic-blocking drugs that do not directly
affect CBF might be preferable to drugs that are
potential cerebral vasodilators. Typically, large
doses of esmolol as a 1 mg/kg bolus followed by an
infusion of approximately 0.5 mg/kg/minute are
required in these patients. Supplemental labetalol
might also be needed during the infusion of esmolol.
Drugs such as sodium nitroprusside and nitroglycerin
may also be used. Because hypotension may cause
nausea and vomiting, supplemental doses of
antiemetic drugs such as droperidol, 1.25 mg; ondansetron, 4 mg;
or dolasetron, 12.5 mg, may be given before
decreasing the blood pressure.
Deliberate hypotension. Two primary indications for
deliberate hypotension are to decrease blood flow
through an arteriovenous fistula during the
injection of glue and to test the cerebrovascular
reserve of the patient undergoing carotid occlusion.
In most instances, the level of sedation is
decreased to permit neurologic examination during
the period of deliberate hypotension. The induction
of hypotension in awake or minimally sedated
patients can be fairly challenging because large
doses of hypotensive drugs may be required to reduce
the blood pressure in these patients.
Adrenergic-blocking drugs that do not directly
affect CBF might be preferable to drugs that are
potential cerebral vasodilators. Typically, large
doses of esmolol as a 1 mg/kg bolus followed by an
infusion of approximately 0.5 mg/kg/minute are
required in these patients. Supplemental labetalol
might also be needed during the infusion of esmolol.
Drugs such as sodium nitroprusside and nitroglycerin
may also be used. Because hypotension may cause
nausea and vomiting, supplemental doses of
antiemetic drugs such as droperidol, 1.25 mg; ondansetron, 4 mg;
or dolasetron, 12.5 mg, may be given before
decreasing the blood pressure.
 Flow arrest. Transient flow arrest has been used
successfully for treating high-flow cerebral AVMs in
relatively healthy (American Society of
Anesthesiologists [ASA] status I and II) patients
with the embolization of NBCA glue. When flow arrest
is planned, the patient is prepared for a general
anesthetic. In addition to the usual preparation, a
central venous catheter is inserted to inject drugs.
Intravenous adenosine as a 10 to 90 mg bolus has
been used for this purpose. Either external pacing
pads or a transvenous pacing line is inserted for
treating any persistent arrhythmias. The procedure
is generally conducted in two parts. In the first
part, the target feeding artery is identified and
the safety of embolizing the vessel is assessed by
performing a superselective Wada test under minimum
alveolar concentration sedation. In the second part
with the catheter positioned in the desired
location, general anesthesia is induced. Conducting
a dose-response study to determine the optimal dose
of adenosine is recommended. The dose of intravenous
adenosine is geared to produce 5 to 15 seconds of
asystole and ranges from 10 to 90 mg. Small amounts
of either esmolol or nitroprusside might be
necessary to treat rebound hypertension or
tachycardia.
Flow arrest. Transient flow arrest has been used
successfully for treating high-flow cerebral AVMs in
relatively healthy (American Society of
Anesthesiologists [ASA] status I and II) patients
with the embolization of NBCA glue. When flow arrest
is planned, the patient is prepared for a general
anesthetic. In addition to the usual preparation, a
central venous catheter is inserted to inject drugs.
Intravenous adenosine as a 10 to 90 mg bolus has
been used for this purpose. Either external pacing
pads or a transvenous pacing line is inserted for
treating any persistent arrhythmias. The procedure
is generally conducted in two parts. In the first
part, the target feeding artery is identified and
the safety of embolizing the vessel is assessed by
performing a superselective Wada test under minimum
alveolar concentration sedation. In the second part
with the catheter positioned in the desired
location, general anesthesia is induced. Conducting
a dose-response study to determine the optimal dose
of adenosine is recommended. The dose of intravenous
adenosine is geared to produce 5 to 15 seconds of
asystole and ranges from 10 to 90 mg. Small amounts
of either esmolol or nitroprusside might be
necessary to treat rebound hypertension or
tachycardia.
 Deliberate hypertension. During the occlusion of a
cerebral artery, planned or inadvertent, systemic
blood pressure might need to be increased to augment
CBF through collateral vessels. The extent to which
the blood pressure needs to be increased depends on
the condition of the patient and the nature of the
disease. During deliberate hypertension, the
systemic blood pressure typically is raised either
to 30% to 40% above the patient's baseline or until
the ischemic symptoms resolve. The electrocardiogram
and ST segments should be inspected for myocardial
ischemia. Phenylephrine is the first-line drug for
deliberate hypertension. Dopamine might be useful in
patients who have a low heart rate.
Deliberate hypertension. During the occlusion of a
cerebral artery, planned or inadvertent, systemic
blood pressure might need to be increased to augment
CBF through collateral vessels. The extent to which
the blood pressure needs to be increased depends on
the condition of the patient and the nature of the
disease. During deliberate hypertension, the
systemic blood pressure typically is raised either
to 30% to 40% above the patient's baseline or until
the ischemic symptoms resolve. The electrocardiogram
and ST segments should be inspected for myocardial
ischemia. Phenylephrine is the first-line drug for
deliberate hypertension. Dopamine might be useful in
patients who have a low heart rate.
Deliberate hypercapnia. Deliberate hypercapnia to a
Paco2 of 50 to 60 mm Hg may be induced during the
treatment of venous malformations of the head and
neck. The rationale for employing hypercapnia is to
increase cerebral venous outflow relative to
extracranial venous drainage and to create a
pressure gradient that would divert sclerosing
agents away from the intracranial veins. This is
usually achieved by decreasing minute ventilation.
Alternatively, CO2 may be added to the inspired
gases.
 Radiation safety. The INR suite has three sources of
radiation: direct radiation (from the x-ray tub),
leakage (through the collimator's protective
shielding), and scattered (or reflected from the
patient and the area surrounding the body part being
imaged). It
is important to realize that the amount of exposure
drops proportionally to the square of the distance
from the source of radiation (inverse square law).
It should also be realized that DSA delivers
considerably more radiation than fluoroscopy.
Everyone working in the INR suite must wear a lead
apron, a thyroid shield, and a radiation exposure
badge. Although they are heavy, using leaded glasses
is a consideration for anyone who must be near the
source of the radiation.
Radiation safety. The INR suite has three sources of
radiation: direct radiation (from the x-ray tub),
leakage (through the collimator's protective
shielding), and scattered (or reflected from the
patient and the area surrounding the body part being
imaged). It
is important to realize that the amount of exposure
drops proportionally to the square of the distance
from the source of radiation (inverse square law).
It should also be realized that DSA delivers
considerably more radiation than fluoroscopy.
Everyone working in the INR suite must wear a lead
apron, a thyroid shield, and a radiation exposure
badge. Although they are heavy, using leaded glasses
is a consideration for anyone who must be near the
source of the radiation.
IV. Management of procedural catastrophes Complications arising from cerebrovascular
instrumentation can be rapid and dramatic and
require a multidisciplinary approach to management.
A catastrophe plan such as that shown in Table-1
should be clearly defined by the anesthesia team for
every INR procedure. Drugs and equipment required to
secure the airway must be available without any
delay. Protamine should be available for immediate
injection if the decision is made to reverse the
heparinization. There must be effective
communication between the INR team and the
anesthesiologist. The appropriate neurologic and
neurosurgical consultants should be contacted as
soon as possible. The anesthesia team has the
primary responsibility to secure the airway and
ensure adequate ventilation. While securing the
airway, the anesthesiologist must communicate with
the INR team to determine whether the problem is
occlusive or hemorrhagic.
|
Table-1. Management of neurologic catastrophesa
|
| Initial resuscitation: Communicate with
radiologists. Call for assistance. Secure the airway
and hyperventilate with 100% O2. Determine if
problem is hemorrhagic or occlusive. |
| Hemorrhagic: Immediate heparin reversal (1 mg
protamine for each 100 U heparin given) and
low-normal pressure. |
| Occlusive: Deliberate hypertension, titrated to
neurologic examination, angiography, or physiologic
imaging studies (e.g., TCD, CBF). |
| Further resuscitation: Head-up 15� in neutral
position. Titrate ventilation to a PaCO2 of 26 to 28
mm Hg. Give 0.5 g/kg mannitol, rapid intravenous
infusion. Anticonvulsants: phenytoin (give slowly,
50 mg/min) and phenobarbital. Titrate thiopental
infusion to electroencephalogram burst suppression.
Allow body temperature to fall as quickly as
possible to 33�C to 34�C. Consider dexamethasone
10 mg.b |
a These are only general recommendations, and drug
doses must be adapted to specific clinical
situations and in accordance with a patient's
preexisting medical condition. In some cases of
asymptomatic or minor vessel puncture or occlusion,
less aggressive management might be appropriate.
bSteroids are of dubious value in the treatment of
focal cerebral ischemia but might have a place in
reducing mass effect from a hemorrhage, if
clinically appropriate.
TCD, transcranial Doppler; CBF, cerebral blood flow. |
 Occlusive catastrophes. In the case of vascular
occlusion, the primary strategy is to increase
distal cerebral perfusion either by augmentation of
the blood pressure or by thrombolysis. Both
therapies may be combined.
Occlusive catastrophes. In the case of vascular
occlusion, the primary strategy is to increase
distal cerebral perfusion either by augmentation of
the blood pressure or by thrombolysis. Both
therapies may be combined.
 Bleeding catastrophes
may be heralded by headache,
nausea, vomiting, and vascular pain related to the
area of the vascular perforation. The radiologist
might see extravasation of the contrast only seconds
before the patient becomes symptomatic. In the case
of the puncture of a vessel, reversal of the heparin
before withdrawing either the offending wire or the
catheter back into the lumen of the vessel keeps the
perforation partially occluded until hemostatic
function has been restored. Immediate reversal of
heparin is indicated as soon as an intracranial
hemorrhage has been diagnosed. Protamine, 1 mg for
every 100 U of heparin given, is administered
without undue regard for systemic blood pressure. An
ACT may be obtained later to adjust the final dose.
When active bleeding occurs, the blood pressure must
be kept as low as possible. Once the bleeding has
been controlled, the target blood pressure should be
discussed with the INR team. If vascular occlusion
has been used to control the hemorrhage, the INR
team may request deliberate hypertension. Allergic
reactions to protamine are rare but can occur.
Bleeding catastrophes
may be heralded by headache,
nausea, vomiting, and vascular pain related to the
area of the vascular perforation. The radiologist
might see extravasation of the contrast only seconds
before the patient becomes symptomatic. In the case
of the puncture of a vessel, reversal of the heparin
before withdrawing either the offending wire or the
catheter back into the lumen of the vessel keeps the
perforation partially occluded until hemostatic
function has been restored. Immediate reversal of
heparin is indicated as soon as an intracranial
hemorrhage has been diagnosed. Protamine, 1 mg for
every 100 U of heparin given, is administered
without undue regard for systemic blood pressure. An
ACT may be obtained later to adjust the final dose.
When active bleeding occurs, the blood pressure must
be kept as low as possible. Once the bleeding has
been controlled, the target blood pressure should be
discussed with the INR team. If vascular occlusion
has been used to control the hemorrhage, the INR
team may request deliberate hypertension. Allergic
reactions to protamine are rare but can occur.
V. Postprocedural considerations Patients are usually observed in the intensive care
unit for the first 24 hours after intracranial and
spinal procedures. The groin is monitored for
bleeding from the femoral puncture site. In general,
INR procedures have their own inherent potential
complications and require frequent neurologic,
metabolic, and hemodynamic monitoring. For example,
after embolization of an AVM, the tissue edema might
be minimal but still sufficient to cause
deterioration in the patient's neurologic status
during the course of the first evening after the
procedure.
VI. Specific procedures
 Superselective anesthesia and functional examination
(SAFE) or superselective Wada is routinely performed
before therapeutic embolization to minimize the risk
of occluding a nutritive vessel to eloquent regions
of either the brain or the spinal cord. This could
happen if the microcatheter tip is proximal to the
origin of the nutritive vessel. Not all interventionalists, however, recognize the need for
SAFE before embolization. The level of sedation is
decreased before testing by discontinuing the
infusion of propofol. In rare instances, it might be
necessary to use naloxone or flumazenil to
antagonize other intravenous drugs. The INR team
performs a baseline focused neurologic examination
under residual light sedation.
Superselective anesthesia and functional examination
(SAFE) or superselective Wada is routinely performed
before therapeutic embolization to minimize the risk
of occluding a nutritive vessel to eloquent regions
of either the brain or the spinal cord. This could
happen if the microcatheter tip is proximal to the
origin of the nutritive vessel. Not all interventionalists, however, recognize the need for
SAFE before embolization. The level of sedation is
decreased before testing by discontinuing the
infusion of propofol. In rare instances, it might be
necessary to use naloxone or flumazenil to
antagonize other intravenous drugs. The INR team
performs a baseline focused neurologic examination
under residual light sedation.
Sodium amobarbital, 30 mg/mL, or lidocaine, 30
mg/mL, mixed with contrast is injected through
the superselective catheter to obtain an angiogram
with the drug/contrast mixture. Sodium amobarbital
is used to investigate the gray matter. Lidocaine
can be used to evaluate the integrity of the white
matter tracts, especially in the spinal cord. The
injection of lidocaine into cortical areas,
particularly those close to the motor strip, can
precipitate seizures, however. Such seizure activity
can cause transient neurologic deficits. Postictal
paralysis may also confuse the interpretation of the
test. For this reason, the barbiturate is usually
given first, followed by lidocaine. If the
amobarbital test is negative, the amobarbital can
protect against seizures but will not interfere with
the assessment of lidocaine's effect on white matter
tracts.
 Superselective angiography and therapeutic
embolization of AVMs. Typically, patients who
present for embolization have large, complex, parenchymatous AVMs, which are composed of several
discrete fistulae with multiple feeding arteries.
The goal of the therapeutic embolization is to
obliterate as many of the fistulae as possible. The
procedure can last up to 4 to 5 hours, depending on
the complexity of the lesion. Various embolic
materials have been used to obliterate AVM fistulae
including polyvinyl chloride particles. More durable
results have been achieved with NBCA glue.
Superselective angiography and therapeutic
embolization of AVMs. Typically, patients who
present for embolization have large, complex, parenchymatous AVMs, which are composed of several
discrete fistulae with multiple feeding arteries.
The goal of the therapeutic embolization is to
obliterate as many of the fistulae as possible. The
procedure can last up to 4 to 5 hours, depending on
the complexity of the lesion. Various embolic
materials have been used to obliterate AVM fistulae
including polyvinyl chloride particles. More durable
results have been achieved with NBCA glue.
In rare cases, INR treatment is aimed at total
obliteration. More commonly, however, embolization
is employed as an adjunct in preparation for either
surgery or radiotherapy and can be beneficial in
several ways. First, embolization may facilitate
operation by obliterating deep feeding arteries that
are difficult to approach surgically and thereby
reduce the surgical risk. Second, staging the
obliteration of the arteriovenous shunts also
theoretically allows the surrounding brain to
accommodate to the alterations in hemodynamics and
may prevent normal perfusion-pressure breakthrough.
Third, the obliteration of high-flow feeders can
benefit patients who have either progressive
neurologic deficits or intractable seizures.
Neurologic improvement after high-flow AVM
embolization has been attributed to the decease in
cerebral steal and a decrease in the mass of the
lesion. Finally, approximately 10% of patients with
AVM harbor intracranial aneurysms. Such aneurysms
appear to increase the risk of spontaneous
hemorrhage from AVMs. The obliteration of intranidal
aneurysms during the initial embolization may
decrease the rate of recurrent hemorrhage during the
course of treatment.
Once the catheter has been positioned for potential
glue injection, SAFE is performed. If SAFE is
positive (i.e., if focal neurologic deficits
develop), either the catheter is repositioned or
embolization of that pedicle is aborted. If the test
is negative, either glue or
another embolic material may be injected. Controlled
deposition of the glue is necessary to decrease
complications from pulmonary embolism or obstruction
of the AVM's venous drainage. The achievement of
flow arrest through the fistula is necessary during
injection of the glue to facilitate polymerization
and solidification of NBCA glue. Techniques for flow
arrest include deliberate hypotension, balloon
occlusion of the proximal vessel, and circulatory
pause with either adenosine or controlled
ventricular fibrillation. In most instances,
deliberate hypotension suffices for flow arrest,
which can be achieved when the mean systemic blood
pressure is reduced to approximately 50 mm Hg. Flow
arrest is usually not needed for embolization with
PVA particles.
The measurement of the immediate postembolization
pressure has been suggested as a way to follow the
course of hemodynamic changes and predict
postprocedure complications. A large increase in the
pressure of the feeding artery after embolization
may be associated with intracranial hemorrhage.
Because the AVM's feeding arteries supply normal
vascular territories to a variable degree, the
abrupt restoration of normal perfusion pressure to a
chronically hypotensive vascular bed might overwhelm
its autoregulatory capacity and result in either
hemorrhage or swelling, the phenomenon known as
normal perfusion-pressure breakthrough. For this
reason, the target range for maintenance of
posttreatment blood pressure is at or slightly below
the normal blood pressure of the patient.
 Embolization of spinal cord lesions.
Embolization can be used to treat intramedullary
spinal AVMs, dural fistulae, and tumors invading the
spinal canal. For cases performed under general
anesthesia with endotracheal intubation, an
intraoperative "wake-up
test"� may be requested. The wake-up test must be
explained to the patient the night before and on the
day of surgery. A N2O/narcotic anesthetic technique
with concurrent administration of propofol may be
employed for the procedure. Neuromuscular blockade,
if required, should be readily reversible for the
wake-up test. For selected lesions, somatosensory
and motor evoked potentials may be helpful in both
anesthetized and sedated patients. When motor evoked
potentials are monitored, the degree of
neuromuscular blockade should be titrated to the
monitoring needs.
Embolization of spinal cord lesions.
Embolization can be used to treat intramedullary
spinal AVMs, dural fistulae, and tumors invading the
spinal canal. For cases performed under general
anesthesia with endotracheal intubation, an
intraoperative "wake-up
test"� may be requested. The wake-up test must be
explained to the patient the night before and on the
day of surgery. A N2O/narcotic anesthetic technique
with concurrent administration of propofol may be
employed for the procedure. Neuromuscular blockade,
if required, should be readily reversible for the
wake-up test. For selected lesions, somatosensory
and motor evoked potentials may be helpful in both
anesthetized and sedated patients. When motor evoked
potentials are monitored, the degree of
neuromuscular blockade should be titrated to the
monitoring needs.
 Carotid test occlusion and therapeutic carotid
occlusion. Test occlusion of the carotid artery is
undertaken either before the anticipated sacrifice
of the vessel or when temporary carotid occlusion
may be required during surgery. During the test
occlusion, a catheter with a distal balloon and a
lumen is placed in the ICA. A baseline neurologic
examination is performed. Flow velocity is measured
over the middle cerebral artery by TCD ultrasound,
if available,
and the CBF can be measured by the intracarotid 133Xe injection technique. Baseline femoral and
carotid artery pressures are also noted. The balloon
is then inflated and the pressure in the carotid
artery distal to the balloon is recorded. The
inflation of the balloon can cause headache and at
times an increase in the systemic blood pressure.
Aggressive treatment of the hypertension is probably
not warranted because it may decrease collateral
perfusion pressure. The anesthesiologist should be
prepared to treat bradycardia with atropine. The
neurologic examination is repeated a few minutes
after occlusion, and TCD and 133Xe CBF measurements
are taken again. After 133Xe washout data have been
obtained, a radioactive tracer for single-photon
emission computerized tomography (SPECT) studies may
be injected. This provides a snapshot measurement of
regional CBF during ICA occlusion. Because SPECT
tracers usually have a long half-life and bind
avidly to cerebral tissues, the imaging part of a
SPECT study may be undertaken in the nuclear
medicine department after the patient leaves the INR
suite.
Carotid test occlusion and therapeutic carotid
occlusion. Test occlusion of the carotid artery is
undertaken either before the anticipated sacrifice
of the vessel or when temporary carotid occlusion
may be required during surgery. During the test
occlusion, a catheter with a distal balloon and a
lumen is placed in the ICA. A baseline neurologic
examination is performed. Flow velocity is measured
over the middle cerebral artery by TCD ultrasound,
if available,
and the CBF can be measured by the intracarotid 133Xe injection technique. Baseline femoral and
carotid artery pressures are also noted. The balloon
is then inflated and the pressure in the carotid
artery distal to the balloon is recorded. The
inflation of the balloon can cause headache and at
times an increase in the systemic blood pressure.
Aggressive treatment of the hypertension is probably
not warranted because it may decrease collateral
perfusion pressure. The anesthesiologist should be
prepared to treat bradycardia with atropine. The
neurologic examination is repeated a few minutes
after occlusion, and TCD and 133Xe CBF measurements
are taken again. After 133Xe washout data have been
obtained, a radioactive tracer for single-photon
emission computerized tomography (SPECT) studies may
be injected. This provides a snapshot measurement of
regional CBF during ICA occlusion. Because SPECT
tracers usually have a long half-life and bind
avidly to cerebral tissues, the imaging part of a
SPECT study may be undertaken in the nuclear
medicine department after the patient leaves the INR
suite.
To assess the patient's cerebrovascular reserve, the
systemic blood pressure can be decreased if the
patient has not demonstrated any neurologic
impairment during the initial ICA occlusion. The
neurologic examination is repeated at frequent
intervals while the blood pressure is reduced. The
distal ICA or stump pressure at which neurologic
deterioration occurs and whether the patient starts
yawning "often a sign of impending cerebral ischemia" are noted and correlated with the
corresponding TCD flow velocity. Depending on the
clinical condition of the patient, another 133Xe
measurement is obtained. If overt neurologic
symptoms develop, the balloon is immediately
deflated, hypotensive drugs are discontinued, and
vasopressors might be required to increase the blood
pressure to normal levels, depending on the clinical
situation.
Although uniform guidelines for interpreting the
results of test occlusion are yet to be formulated,
a new neurologic deficit, significant asymmetry on
SPECT imaging, and a 25% to 30% reduction in CBF as
measured after occlusion by either 133Xe CBF or TCD
may be considered as relative indications for an
extracranial to intracranial bypass procedure before
sacrifice of the carotid artery.
 Aneurysm ablation. Many intracranial aneurysms are
amenable to endovascular treatment. As the
techniques of interventional therapy have continued
to evolve, endovascular ablation is increasingly
considered to be the primary treatment modality for
ruptured and unruptured intracranial aneurysms. The
indications for open surgical versus endovascular
therapy are currently a topic of vigorous
discussion. There
are two basic approaches for endovascular
obliteration of intracranial aneurysms: (a) the
occlusion of the proximal parent artery, such as the
carotid artery, which was discussed earlier and (b)
obliteration of the aneurysmal sac itself.
Endovascular obliteration of the aneurysmal sac is
usually accomplished through the use of detachable
coils manufactured by a wide variety of vendors.
Complicated aneurysms that have wide necks and large
sacs may require advanced techniques involving
either temporary balloon remodeling or placing an
intracranial stent. These procedures may be
prolonged and require general anesthesia with
endotracheal intubation. The anesthesiologist should
be prepared for the occurrence of aneurysmal
subarachnoid hemorrhage (SAH) either spontaneously
or as a result of the intravascular manipulations.
Occlusive complications may also develop and require
additional maneuvers to enhance CBF and initiate
revascularization. Occlusion and thrombosis of the
aneurysm may be ongoing immediately after
intervention. Therefore, careful attention to the
control of blood pressure in the postprocedure
period remains critical, especially in patients who
have presented with SAH.
Aneurysm ablation. Many intracranial aneurysms are
amenable to endovascular treatment. As the
techniques of interventional therapy have continued
to evolve, endovascular ablation is increasingly
considered to be the primary treatment modality for
ruptured and unruptured intracranial aneurysms. The
indications for open surgical versus endovascular
therapy are currently a topic of vigorous
discussion. There
are two basic approaches for endovascular
obliteration of intracranial aneurysms: (a) the
occlusion of the proximal parent artery, such as the
carotid artery, which was discussed earlier and (b)
obliteration of the aneurysmal sac itself.
Endovascular obliteration of the aneurysmal sac is
usually accomplished through the use of detachable
coils manufactured by a wide variety of vendors.
Complicated aneurysms that have wide necks and large
sacs may require advanced techniques involving
either temporary balloon remodeling or placing an
intracranial stent. These procedures may be
prolonged and require general anesthesia with
endotracheal intubation. The anesthesiologist should
be prepared for the occurrence of aneurysmal
subarachnoid hemorrhage (SAH) either spontaneously
or as a result of the intravascular manipulations.
Occlusive complications may also develop and require
additional maneuvers to enhance CBF and initiate
revascularization. Occlusion and thrombosis of the
aneurysm may be ongoing immediately after
intervention. Therefore, careful attention to the
control of blood pressure in the postprocedure
period remains critical, especially in patients who
have presented with SAH.
 Angioplasty. Either mechanical angioplasty or
pharmacologic dilatation may be indicated for
vasospasm after SAH and for atherosclerotic
cerebrovascular disease.
Angioplasty. Either mechanical angioplasty or
pharmacologic dilatation may be indicated for
vasospasm after SAH and for atherosclerotic
cerebrovascular disease.
 Angioplasty for cerebral vasospasm is usually
undertaken in patients who, despite maximum medical
management, continue to demonstrate neurologic signs
and symptoms of cerebral ischemia. These patients
are often in extremis: their tracheas are frequently
intubated, they are receiving vasopressor drugs, and
they have either an external ventricular drain or
other device in place to monitor intracranial
pressure. Angiography is first undertaken to
demonstrate that a significant degree of spasm in
large proximal vessels (anterior, middle, and
posterior cerebral arteries) exists. A balloon
catheter is guided under fluoroscopy into the
spastic segment and inflated to distend the
constricted area mechanically. If deliberate
hypertension is being used to ameliorate a focal
neurologic deficit before angioplasty, the blood
pressure should be reduced to the patient's normal
range after angiographic demonstration of
significant widening of the spastic segment.
Angioplasty for cerebral vasospasm is usually
undertaken in patients who, despite maximum medical
management, continue to demonstrate neurologic signs
and symptoms of cerebral ischemia. These patients
are often in extremis: their tracheas are frequently
intubated, they are receiving vasopressor drugs, and
they have either an external ventricular drain or
other device in place to monitor intracranial
pressure. Angiography is first undertaken to
demonstrate that a significant degree of spasm in
large proximal vessels (anterior, middle, and
posterior cerebral arteries) exists. A balloon
catheter is guided under fluoroscopy into the
spastic segment and inflated to distend the
constricted area mechanically. If deliberate
hypertension is being used to ameliorate a focal
neurologic deficit before angioplasty, the blood
pressure should be reduced to the patient's normal
range after angiographic demonstration of
significant widening of the spastic segment.
 Pharmacologic dilatation is also used for the
treatment of cerebral vasospasm by direct
intra-arterial injection of vasodilators under
fluoroscopic guidance. Although the technique was
originally described for papaverine, the selection
of vasodilators has now expanded to include the more
frequent use of calcium-channel-blocking
drugs such as verapamil and nicardipine. During
recirculation, the anesthesiologist needs to monitor
for systemic side effects of these drugs, which
include hypotension and bradycardia, especially with
the calcium-channel-blocking drugs.
Pharmacologic dilatation is also used for the
treatment of cerebral vasospasm by direct
intra-arterial injection of vasodilators under
fluoroscopic guidance. Although the technique was
originally described for papaverine, the selection
of vasodilators has now expanded to include the more
frequent use of calcium-channel-blocking
drugs such as verapamil and nicardipine. During
recirculation, the anesthesiologist needs to monitor
for systemic side effects of these drugs, which
include hypotension and bradycardia, especially with
the calcium-channel-blocking drugs.
 Angioplasty for atherosclerosis.
At present, patients who have high-risk factors for
carotid endarterectomy are considered favorable
candidates for cervical carotid angioplasty and
stenting (CAS, Stenting and Angioplasty with
Protection in Patients at High Risk for
Endarterectomy [SAPPHIRE] Trial). Studies evaluating
the safety and efficacy of carotid stenting in
traditional "low-risk"�
patients are ongoing (Carotid Revascularization
Endarterectomy versus Stent Trial [CREST]), with
encouraging preliminary results. These patients
generally require balloon dilatation and placement
of a vascular stent. In many cases, the insertion of
a cerebroprotective device may be used to decrease
the risk of distal thromboembolism. Angioplasty of
the ICA is usually undertaken with minimal sedation.
General anesthesia is required for treating segments
of the intracranial arteries. Intracranial
angioplasty and stenting procedures for
atherosclerosis have a higher level of risk
secondary to the inherently more delicate nature of
intracranial vessels. Intracranial arteries have a
thinner media and therefore are more prone to
dissection and perforation. The selection of
anesthetic technique also depends on the patient's
medical condition and ability to cooperate during
the procedure as well as the presence of anticipated
technical difficulty in negotiating the stenosed
segment. Deliberate hypertension may be required to
augment collateral blood flow. The considerations
for general anesthesia are similar to those for
carotid endarterectomy.
Angioplasty for atherosclerosis.
At present, patients who have high-risk factors for
carotid endarterectomy are considered favorable
candidates for cervical carotid angioplasty and
stenting (CAS, Stenting and Angioplasty with
Protection in Patients at High Risk for
Endarterectomy [SAPPHIRE] Trial). Studies evaluating
the safety and efficacy of carotid stenting in
traditional "low-risk"�
patients are ongoing (Carotid Revascularization
Endarterectomy versus Stent Trial [CREST]), with
encouraging preliminary results. These patients
generally require balloon dilatation and placement
of a vascular stent. In many cases, the insertion of
a cerebroprotective device may be used to decrease
the risk of distal thromboembolism. Angioplasty of
the ICA is usually undertaken with minimal sedation.
General anesthesia is required for treating segments
of the intracranial arteries. Intracranial
angioplasty and stenting procedures for
atherosclerosis have a higher level of risk
secondary to the inherently more delicate nature of
intracranial vessels. Intracranial arteries have a
thinner media and therefore are more prone to
dissection and perforation. The selection of
anesthetic technique also depends on the patient's
medical condition and ability to cooperate during
the procedure as well as the presence of anticipated
technical difficulty in negotiating the stenosed
segment. Deliberate hypertension may be required to
augment collateral blood flow. The considerations
for general anesthesia are similar to those for
carotid endarterectomy.
 Thrombolysis for acute stroke. It is possible to recanalize the occluded vessel after an acute
thromboembolic stroke by either mechanical means or
superselective intra-arterial delivery of
thrombolytic agents, such as recombinant tissue
plasminogen activator, streptokinase, or urokinase.
Significant improvement in neurologic outcome has
been demonstrated when either pharmacologic
thrombolysis is completed within 6 hours of the
onset of ischemic symptoms (Prolyse in Acute
Cerebral Thromboembolism II [PROACT II]) or
mechanical thrombolysis is performed within 8 hours
(Mechanical Embolus Removal in Cerebral Ischemia
[MERCI] Trial). Techniques for mechanical means of
clot retrieval, balloon angioplasty, and laser
ablation are also being developed. These methods can
restore arterial flow more rapidly than
intra-arterial thrombolysis, which may
require up to 2 hours. In the vertebro-basilar
circulation, treatment may be effective even when
administered as long as 24 hours after the onset of
symptoms. The main risk of intra-arterial
thrombolysis is hemorrhagic conversion of the
ischemic infarct, which has a high mortality when it
occurs.
Thrombolysis for acute stroke. It is possible to recanalize the occluded vessel after an acute
thromboembolic stroke by either mechanical means or
superselective intra-arterial delivery of
thrombolytic agents, such as recombinant tissue
plasminogen activator, streptokinase, or urokinase.
Significant improvement in neurologic outcome has
been demonstrated when either pharmacologic
thrombolysis is completed within 6 hours of the
onset of ischemic symptoms (Prolyse in Acute
Cerebral Thromboembolism II [PROACT II]) or
mechanical thrombolysis is performed within 8 hours
(Mechanical Embolus Removal in Cerebral Ischemia
[MERCI] Trial). Techniques for mechanical means of
clot retrieval, balloon angioplasty, and laser
ablation are also being developed. These methods can
restore arterial flow more rapidly than
intra-arterial thrombolysis, which may
require up to 2 hours. In the vertebro-basilar
circulation, treatment may be effective even when
administered as long as 24 hours after the onset of
symptoms. The main risk of intra-arterial
thrombolysis is hemorrhagic conversion of the
ischemic infarct, which has a high mortality when it
occurs.
Anesthetic considerations in these patients include
those for elderly people and for patients who have
widespread arterial disease. Hypertension occurs
spontaneously after acute thromboembolic stroke and,
in the face of nonhemorrhagic focal neurologic
deficits, should not be treated aggressively. Once
clot lysis has been accomplished, the blood pressure
is maintained in the patient's normal range and
ideally titrated to some index of CBF to prevent
hyperperfusion injury.
 Treatment of other CNS vascular malformations
Treatment of other CNS vascular malformations
 Dural AVMs. Dural AVMs induce venous hypertension,
and, when cortical venous drainage is involved, may
cause intracranial hemorrhage. Multiple intracranial
and extracranial arteries may feed these dural AVMs
so that multistage embolization is usually
performed. SAFE are required, as in the case of
intracranial AVMs. Transarterial embolization with
NBCA glue is a commonly utilized technique, as is
the transvenous coil occlusion of pathologic venous
pouches.
Dural AVMs. Dural AVMs induce venous hypertension,
and, when cortical venous drainage is involved, may
cause intracranial hemorrhage. Multiple intracranial
and extracranial arteries may feed these dural AVMs
so that multistage embolization is usually
performed. SAFE are required, as in the case of
intracranial AVMs. Transarterial embolization with
NBCA glue is a commonly utilized technique, as is
the transvenous coil occlusion of pathologic venous
pouches.
 Carotid cavernous fistulae. Skull-base trauma is the
most common etiology of carotid cavernous fistula.
Traumatic fistulae can also occur between the
vertebral artery and the paravertebral veins. Such
arteriovenous fistulae can lead to chronic
hypotension of the surrounding normal vascular
territories. The treatment may include either transarterial occlusion with detachable balloons or
transvenous occlusion of the involved cavernous
sinus. The obliteration of these fistulae might
result in normal perfusion-pressure breakthrough.
Therefore, after obliterating these lesions, the
blood pressure should be maintained in the range of
10% to 20% below the normal pressure of the patient.
Carotid cavernous fistulae. Skull-base trauma is the
most common etiology of carotid cavernous fistula.
Traumatic fistulae can also occur between the
vertebral artery and the paravertebral veins. Such
arteriovenous fistulae can lead to chronic
hypotension of the surrounding normal vascular
territories. The treatment may include either transarterial occlusion with detachable balloons or
transvenous occlusion of the involved cavernous
sinus. The obliteration of these fistulae might
result in normal perfusion-pressure breakthrough.
Therefore, after obliterating these lesions, the
blood pressure should be maintained in the range of
10% to 20% below the normal pressure of the patient.
 Vein of Galen malformations. These relatively
uncommon but complicated lesions usually present in
infancy and childhood. The patients may have
congestive heart failure, intractable seizures,
hydrocephalus, and mental retardation. Several
approaches have been attempted including transarterial and transvenous methods. Concerns
during general anesthesia for INR therapy are the
same as for surgical treatment. In the setting of
congestive heart failure, preexisting right-to-left
shunts, and pulmonary hypertension, a relatively
small glue embolus can be fatal.
Vein of Galen malformations. These relatively
uncommon but complicated lesions usually present in
infancy and childhood. The patients may have
congestive heart failure, intractable seizures,
hydrocephalus, and mental retardation. Several
approaches have been attempted including transarterial and transvenous methods. Concerns
during general anesthesia for INR therapy are the
same as for surgical treatment. In the setting of
congestive heart failure, preexisting right-to-left
shunts, and pulmonary hypertension, a relatively
small glue embolus can be fatal.
 Intra-arterial chemotherapy and embolization of
tumors. Preoperative embolization as a means
of decreasing blood loss during surgery can be
performed for many hypervascular intracranial or
spinal tumors. Paragangliomas can cause
catecholamine release from the tumor during
embolization, and means of treating the ensuing
hypertensive crisis should be at hand.
Superselective administration of chemotherapeutic
agents can also be used for treating neoplasms
refractory to conventional therapy.
Intra-arterial chemotherapy and embolization of
tumors. Preoperative embolization as a means
of decreasing blood loss during surgery can be
performed for many hypervascular intracranial or
spinal tumors. Paragangliomas can cause
catecholamine release from the tumor during
embolization, and means of treating the ensuing
hypertensive crisis should be at hand.
Superselective administration of chemotherapeutic
agents can also be used for treating neoplasms
refractory to conventional therapy.
 Spinal compression fracture therapy. Vertebroplasty
and kyphoplasty procedures involve the
intravertebral body administration of acrylic bone
cement compounds via a percutaneous, often
transpedicular, approach. Many patients report
significant pain relief after these procedures. The
demographics of this population (elderly, frail,
osteoporotic) and prone positioning require extra
care during the preparation process. Most of these
procedures fortunately can be performed and well
tolerated with mild sedation.
Spinal compression fracture therapy. Vertebroplasty
and kyphoplasty procedures involve the
intravertebral body administration of acrylic bone
cement compounds via a percutaneous, often
transpedicular, approach. Many patients report
significant pain relief after these procedures. The
demographics of this population (elderly, frail,
osteoporotic) and prone positioning require extra
care during the preparation process. Most of these
procedures fortunately can be performed and well
tolerated with mild sedation.
VII. Conclusions Interventional neuroradiology offers a new approach
to several intracranial and spinal disorders. To
some extent, the risk/benefit ratio of INR
procedures remains to be elucidated when compared
with traditional surgical approaches. The anesthetic
management of these procedures, while similar to
traditional operative approaches, is beset with
hazards and requires certain accommodations.
|